Abstract

Background: Uncontrolled studies and a case-matched study indicate that clarithromycin might exert synergistic effects in combination with thalidomide or lenalidomide in the treatment of multiple myeloma. Recent cellular studies have shown that the combination of clarithromycin and bortezomib results in increased cytotoxicity compared to bortezomib alone in myeloma cell lines. A possible mechanism underlying this synergistic effect might be simultaneous inhibition of the ubiquitin-proteasome system by bortezomib and the autophagy-lysosome system by clarithromycin resulting in enhanced endoplasmic reticulum stress-mediated apoptosis in myeloma cells (Moriya et al. Int J Oncol 2013).
The Danish Myeloma Study Group (DMSG) initiated the CLAIM trial (NCT02573935), a randomized placebo-controlled phase II study, to investigate the efficacy and safety of clarithromycin in combination with the bortezomib containing VCD regimen.
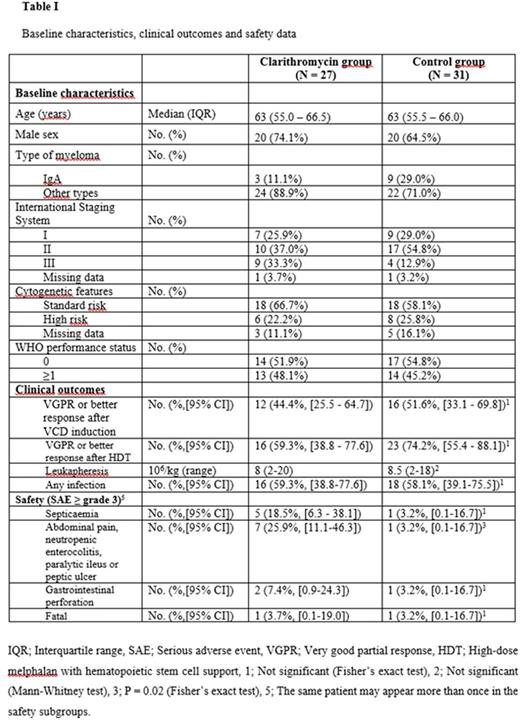
Methods: Patients with newly diagnosed multiple myeloma were randomized (1:1) to receive p.o. clarithromycin 500 mg or a matching placebo tablet twice daily for 63 days in combination with VCD induction therapy. The randomization was stratified according to International Staging System stage. The VCD consisted of 21-day cycles of subcut bortezomib 1.3 mg/sqm days 1, 4, 8, 11, i.v. cyclophosphamide 500 mg/sqm on days 1 and 8, and p.o. dexamethasone 40 mg days 1, 2, 4, 5, 8, 9, 11, 12. After induction treatment the patients proceeded to cyclophosphamide priming (2000 mg/sqm), leukapheresis and high-dose melphalan (200 mg/sqm) with hematopoietic stem cell support (HDT). Patients from six Danish hematology departments participated in the trial. Primary endpoint was to compare rate of very good partial response or better response after three cycles of VCD combined with clarithromycin or placebo. Important secondary end-points were to compare very good partial response or better response two months after HDT, number of stem cells harvested, frequency of infections and safety. The responses were assessed according to the IMWG criteria and analyses were by intention to treat.
Results: The study was prematurely stopped for safety reasons after the inclusion of 58 patients (36% of the planned study population). The enrolled patients were randomly assigned to clarithromycin (27) or placebo (31), and the clinical characteristics at baseline were balanced (Table I). VGPR or better response after the VCD induction therapy was obtained in 12 patients (44.4%, (95% CI, [25.5 - 64.7]) and in 16 patients (51.6%, [33.1 - 69.8], P = 0.59) in the clarithromycin group and the control group, respectively. There was no difference in the secondary endpoints between the treatment groups (Table I). A total of 26 serious adverse events were reported in 16 (59.3%) patients in the clarithromycin group and 16 serious adverse events in 10 (32.3%) patients in the control group. Seven patients (25.9%) in the clarithromycin group developed severe gastrointestinal complications (SAE ≥ grade 3) comprising pain, neutropenic enterocolitis, paralytic ileus or peptic ulcer. These complications occurred in only one patient in the control group (Table I). Septicaemia with Gram negative bacteria was observed in 5 patients in the clarithromycin group. By contrast, the only case of septicaemia detected in the control group was pneumococcal sepsis associated with pneumonia. In consequence of this imbalance in occurrence of severe gastrointestinal symptoms and septicaemia the study safety board decided to stop inclusion of new patients and to stop administration of the study drug on 16 September 2016.
Conclusion: The study was prematurely stopped due to a number of serious adverse events. Although we only could analyse response data in 58 included patients the data do not suggest any effect of clarithromycin when added to the VCD regimen and our trial does not encourage further clinical studies on the combination of clarithromycin and bortezomib. Surprisingly, our study found an increased frequency of serious adverse events, in particular serious gastrointestinal complications and septicaemia, in the clarithromycin group. It emphasizes the need for controlled studies on the effect of clarithromycin, both in assessment of potential anti-myeloma effects as well as assessment of safety measures.
Abildgaard: Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract